The work of community health workers (CHWs), promotores, and other frontline public health workers has become exceptionally critical to improving health and well-being. Yet, unlike other healthcare professionals, CHWs’ expertise isn’t built by educational degrees and clinical licensure. There’s currently no national standard for CHW certification, creating a wide range of challenges for organizations and individual providers interested in elevating person-centered care.
There are, however, several states that have developed their own set of requirements to credential community health professionals, creating standards for work eligibility across care settings, cross-functional provider services, and processes to receive fee-for-service reimbursement, a significant step towards long-term CHW sustainability.
CHW certification and other credentialing standards for Medicaid reimbursement
Community-based organizations and individual CHW providers in 24 states can currently access Medicaid reimbursement, allowing teams to bill for their services. As CHWs are a new provider type, policies have been needed to set reimbursement requirements, manage technical and administrative guidelines, and manage emerging funding pathways.
Consistent across state credentialing standards are some varieties of the CHW Core Consensus (C3) Project’s roles and competencies which may cover the following 10 roles and 11 skills:
Core Roles:
-
Cultural mediation among individuals, communities, and health and social service systems
-
Care coordination, case management, and system Navigation
-
Advocating for individuals and communities
-
Providing direct services
-
Conducting outreach
-
Providing culturally appropriate health education and information
-
Providing coaching and social support
-
Building individual and community capacity
-
Implementing individual and community assessments
-
Participating in evaluation and research
Core Skills:
-
Communication skills
-
Interpersonal and relationship-building skills
-
Service coordination and navigation skills
-
Capacity-building skills
-
Advocacy skills
-
Building individual and community capacity
-
Individual and community assessment
-
Outreach skills
-
Professional skills and conduct
-
Evaluation and research skills
-
Knowledge base
Other requirements may include the successful completion of a designated or pre-approved training program and field experience, a set number of hours of work or volunteer experience, and ancillary certifications, such as mental health first aid. Each state that certifies CHWs go about it differently, but a common theme is that such credentialing is elevating the workforce and enabling further cross-sector care coordination and collaboration.
State Credentialing Examples
California requirements
In California, for example, individuals or volunteers 16 and over (18 and over to qualify for Medi-Cal reimbursement) can become CHW-benefit eligible through the experience or certificate pathway, following the requirements in the Department of Health Care Services’ (DCHS) all-plan letter 24-006.
In the experience pathway, CHWs must:
- Have lived experience in the area they’re providing services (or are highly encouraged to).
- Have at least 2,000 hours working as a CHW in paid or volunteer positions within the previous three years.
In the certificate pathway, CHWs must:
- Self-attest to their lived experience.
- Provide a certificate of completion of a CHW training program no more than five years old.
Volunteers in the state can complete training programs provided by college or university-based programs or community organizations. The entry prices vary dramatically, from no-cost options to programs as high as $3,000.
Regardless of the path, supervising providers must maintain evidence of a CHW’s experience and minimum qualifications through one of the two pathways.
Texas requirements
Although Texas doesn’t reimburse CHW services through its state Medicaid program, volunteers and nonprofit workers can still earn CHW credentials. Applicants must:
- Be 16 years or older.
- Demonstrate eight core competency skills.
- Complete a state-approved 160-hour CHW training program or verify at least 1,000 cumulative hours of community health worker services in the last three years.
In the Lone Star State, experience is limited to work or volunteer experience and not necessarily lived experience.
Rhode Island requirements
Rhode Island is well-known for having a strong CHW network. Any individual certified by the Rhode Island Certification Board (RICB) as a CHW can perform CHW services. And any certified CHW or person who becomes certified within 18 months can get reimbursed for some services through the state’s Medicaid program.
The State of Rhode Island Department of Health lays out a four-step process for becoming a certified CHW:
- Become a member of the Community Health Worker Association of Rhode Island (CHWARI) for free.
- Enroll in CHW training from groups like CHWARI, Clinica Esperanza/Hope Clinic, Community Health Innovations of Rhode Island, and even the Brown University School of Public Health.
- Apply for CHW certification with proof of the following:
- Six months or 1,000 hours of paid or volunteer work experience as a CHW or closely related role within the last five years.
- 50 hours of supervised work in CHW domains.
- 70 hours of education in nine domains:
- Engagement methods and strategies
- Individual and community assessment
- Culturally and linguistically appropriate responsiveness
- Promote health and wellbeing
- Care coordination and system navigation
- Public health concepts and approaches
- Advocacy and community capacity building;
- Safety and self-care
- Ethical responsibilities and professional skills
- Submit a portfolio demonstrating activities and achievements in at least three of the following categories:
- Community experience and involvement
- Research activities
- College-level courses/advanced or specialized training
- Community publications, presentations, and projects
- A statement of professional experience
- Achievements and awards
- Resume or CV
- Performance evaluation
New York requirements
New York offers tailored CHW training programs through organizations, colleges, and universities, but does not require volunteers to be certified to work as CHWs. However, community health worker benefits for certain services are provided based on annual budgets. In cases where nonprofits and CBOs want to get reimbursed for these services, their CHWs must be certified.
For example, in 2023, New York State Medicaid covered CHW services like health advocacy, education, and navigation for pregnant or postpartum women. To qualify for reimbursement, CHWs needed to have or meet the following criteria:
- Have lived experience in pregnancy or birth, housing status, mental health or substance use conditions, or chronic conditions
- Share the race/ethnicity/language/sexual orientation/community of those served
- Complete a minimum of 20 hours of training in CHW core competencies, and/or at least 1,400 hours of work experience as a CHW in formal paid or volunteer roles in the previous three years
- Complete basic HIPAA and mandated reporter training
- Work under the supervision of a Medicaid-enrolled, licensed provider.
The Power of Lived Experience
Finally, and maybe most importantly, state CHW certification and other credentials often require that providers have lived experience.
Lived experience is any knowledge or expertise a CHW gains through their personal identity, culture, or background. Winning a battle with breast cancer, living (or caring for someone) with a disability, recovering from addiction, navigating the immigration system, or overcoming homelessness are all lived experiences that offer insights and empathy that no training can replicate.
Shared lived experiences allow CHWs to break down barriers and connect with their clients, making them especially beneficial to at-risk community members seeking support.
3 ways lived experience improves health outcomes
There are few limits to the kinds of lived experiences that can make a community member or nonprofit worker an effective CHW. Merely sharing a gender identity, sexual orientation, or cultural background with community members qualifies as a lived experience.
Other experiences that allow CHWs to add value to a nonprofit or community-based organization’s (CBO) efforts include:
- Shared race, ethnicity, or cultural origin
- Gender identity
- Sexual orientation
- Language
- Sociodemographic background
- Pregnancy, adoption, and family planning
- Living with a disability
- Incarceration and reentering the community or workforce
- Homelessness or housing insecurity
- Domestic violence or abuse
- Substance use disorder and recovery
- Identifying as a trans or non-binary person
But when it comes down to it, CHWs with lived experience strengthen connection, trust-building, and advocacy between themselves or an organization and clients seeking social or health services.
1. They build trust and rapport with skeptical community members
For community members in the thick of a crisis or other adverse experience, one of the most common obstacles is feeling alone. Some may struggle to seek or accept help, believing professional care providers, even community health workers, CBO staff members, or volunteers can’t relate to them and therefore can’t help.
Let’s say you work to address homelessness and housing insecurity in your community. You likely meet single parents living paycheck-to-paycheck or battling unemployment every day. These clients may initially feel shame or distrust, surrounded by people who are housed or seemingly don’t have to think about where next month’s rent is coming from. This sense of isolation prevents them from opening up or reaching out to your organization.
However, CHWs with lived experience add authenticity, showing community members that their experiences are more universal than they realize and demonstrating a way forward or positive result made possible through education and intervention.
2. They improve patient experience and outcomes
Cultural sensitivity and lived experience can make a significant difference when it comes to helping clients manage disabilities or chronic conditions. Working with CHWs who share conditions as well as cultural, religious, family, or physical attributes with community members can help CBOs and CHWs deliver more effective services.
A 2003 trial studied the effectiveness of diabetes care and control among 186 urban African Americans with type 2 diabetes. Participants were instructed to perform their usual diabetes care on their own, with a nurse case manager, with a CHW, or both.
After two years, the participants who worked with a CHW saw a more significant decline in blood sugar levels compared to those who worked alone. Those who worked with a nurse and a CHW saw improvements in triglycerides and diastolic blood pressure levels compared to those who worked alone.
More recently, a 2023 report uncovered 16 random controlled trials on the impact of CHW intervention on healthcare services in the United States. Five of those trials showed a significant reduction in emergency room visits, hospitalization, or urgent care visits between 20% and 50%. And it further suggests that true connection with CHWs promotes overall health safety.
3. They drive advocacy and policy change
CHWs with lived experience are in the best position to advocate for a client’s needs and affect policy changes that address social drivers of health. Let’s say your CBO works with elderly people in Latinx or Hispanic communities. A CHW with lived experience in similar households or who is Spanish-speaking plays a crucial role in the effectiveness of the organization’s mission.
For one, they can educate clients on the vocabulary and tools they need to advocate for themselves in social or clinical environments. They can also act as translators between clients and medical staff, ensuring better care and health outcomes through clearer communication of treatment plans.
Other CHWs tell their stories in legislative sessions and on social media to advocate for policy changes. In 2023, for example, the nonprofit Partners in Health organized a Congressional briefing to educate lawmakers on the value of CHWs and advocate for the long-term support of the CHW workforce. Organizers visited over 40 Congressional offices to engage in conversation and foster understanding of how CHWs promote health equity.
CHW continued education bridges lived experience and professional development
Along with lived experience, continued education and training can facilitate professional growth and development for new and long-time CHWs and other community-based providers. Training gives CHWs additional tools and resources to leverage their lived experience more effectively and meet requirements for emerging funding pathways, such as Medicaid reimbursement.
There are several avenues for CHWs who want to improve their soft and technical skills. Soft skills may include communication, rapport-building, leadership, public speaking, and conflict management. Technical skills include cultural competency, systems documentation (e.g., utilizing Excel or care coordination software), care planning, and care navigation.
Soft Skills resources
- Partners in Care Foundation for modules on foundational CHW soft and technical skills in education, advocacy, conflict resolution, crisis intervention, and more
- TED Masterclass and Toastmasters for public speaking
- Nonprofitready.org for free leadership training for nonprofit professionals
- Meetup.com for casual community networking, and SCORE.org for more business-first networking
- Local community colleges
Technical Skills resources
- The National Association for Community Health Workers (NACHW) for training programs, events, and peer connection
- State CHW associations, designed to unite and support CHWs with professional development to improve health and health care.
- Public Health Training Center Network courses and events covering current and emerging regional and nationwide topics, cultural competency, and more.
- Think Cultural Health for cultural and linguistic competency training
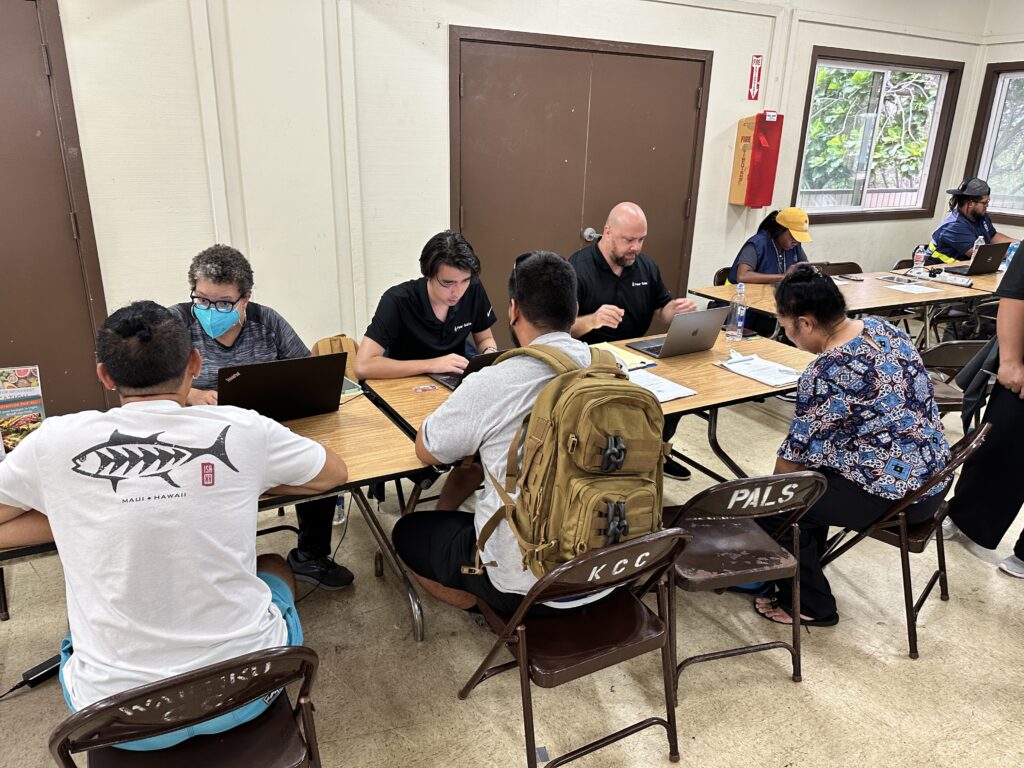
Along with these resources, Pear Suite offers complimentary professional development opportunities for CHWs, both in the care competencies of care navigation and specialized training for technical skills to boost performance, address care gaps, and utilize sustainable revenue sources, like Medicaid reimbursement. Additionally, users of the Pear Suite platform receive ongoing support and training on topics ranging from healthcare compliance, quality improvement, self-care, and hiring and retaining CHWs.
CHW training powered by Pear Suite
We understand that there is currently a lack of high-quality, accessible, and affordable training and development programs, so Pear Suite is working hard to provide free resources and training all year.
In addition to regular webinars taught by industry-leading trainers and experienced CHWs, Pear Suite provides downloadable guides, teaching tools, and funding opportunities across topics and populations of focus, such as domestic violence and LGBTQ+ care, adverse childhood experiences, and more. Additional on-demand resources are also available to CHWs and others who provide community services through the education arm.




