A person’s health is so much more than genes and medical history. Non-medical factors significantly affect everyday quality of life and long-term health outcomes. We call five of those non-medical factors “social drivers of health” (known previously as “structural drivers” and “social determinants”).
The five social drivers, as identified by the U.S. Department of Health and Human Services’ Healthy People 2030 national objectives, include economic stability, access to quality education, access to quality healthcare, built environments, and community context. Read on to learn more about each social driver and how it affects health outcomes, and what community-based organizations (CBOs) are doing to help.
When did “social determinants” become “social drivers” of health? January 2023 marked the unofficial shift from “social determinants” to “social drivers,” as reported by the National Association of Community Health Centers (NACHC). Why “determinants” became “drivers” really comes down to what we believe can and can’t change about what affects a person’s health. A “determinant” decidedly affects the outcome of something. “Drivers,” proponents said, are more flexible and encourage policy-makers, communities, and individuals to be agents of social change. Dr. John W. Hatch, an early adopter of the term, said in a 2023 interview with the NACHC that changing the term “welcomed a different level of conversation” about what it means for communities to play a greater role in health outcomes.
What are social drivers of health?
Social drivers of health are the five non-medical factors that affect your health, everyday well-being, and quality of life. These drivers are present in all areas of your life, from your neighborhood environment to how accessible public transportation is to you.
If you or someone you know has seen a doctor or physician recently, you might have already encountered efforts to promote and address your social drivers of health—and in turn, treat the whole person and not only symptoms. When your intake form addresses questions around your housing and nutrition, for instance, your doctor is assessing what other needs might play into your exam and follow-up care. Healthcare providers who don’t address social drivers of health miss out on opportunities to promote true healing and see higher costs from repeat admissions.
Let’s explore an example.

The man’s doctor prescribes medication to manage his insulin levels. Unfortunately, the family shares a car that can be unreliable, and with work and school schedules, the man frequently misses the pharmacy’s open times and cannot pick up his prescription.
The provider also recommended lifestyle changes, including diet and exercise to help the man manage his diabetes. His job is physical, which provides some activity; however, nutrition is a challenge. Fresh fruits and vegetables can be costly, and since he relies on his family to cook, he often eats options that aren’t aligned with his doctor’s recommendations.
The man and his family do their best to help him follow his care plan, but with limited management, the diabetes worsens, and the man eventually finds himself visiting the emergency department multiple times a year.
Transportation and food access are major drivers here, but that’s just scratching the surface. Each social driver affects another in a seemingly endless cycle.
Economic stability

Economic stability is a social driver of health that encompasses a person’s employment (including work history and turnover), income, expenses, debt (including medical bills and childcare costs), and their ability to access financial support. Too much of one and not enough of another (income and medical bills, for example) can significantly affect a person’s long-term health.
What economic instability looks like in a person’s health
A math tutor loses some of her income when the afterschool program she works at unexpectedly cuts its tutoring program. She teaches some evening classes at the local community college and tutors privately on the weekends, but she is reliant on the insurance and consistent schedule of her employer.
Now, without insurance from her employer, she is worried about the risk that lack of coverage poses for her and her two children, both of whom play sports at their local high school. She also silently worries about affording sports and school fees, groceries, and other expenses, as a single parent.
Access to quality education
Quality education is a social driver of health that encompasses language and literacy and access to early childhood education, vocational training, or higher education. A person’s ability to access quality education for themselves, or their children, follows them throughout their lives, as it affects their ability to understand and navigate social, financial, and professional systems early and later in life.
What lack of quality education looks like in a person’s health
A high school boy who experienced delayed language skills as a child struggles with reading comprehension. As a result, he struggles to follow written instructions, turn in assignments, and maintain his grades. Even positive initiatives around healthy habits, such as the school’s mental health resources fair are inhibited by the boy’s reading abilities.
Shame and anxiety turn to anger and frustration, pushing the student into skipping classes, and leading to truancy. Discouraged, the boy turns to unhealthy coping mechanisms that affect his physical and psychological development. He falls behind and eventually drops out.
Access to quality healthcare
Quality healthcare is a social driver of health encompassing a person’s proximity and access to primary care, specialty providers, and other medical services, such as mental health counseling. It also includes their insurance coverage and copay amounts.
Before the Affordable Care Act (ACA), around 15% of Americans were uninsured. In 2014, provisions of the ACA expanded Medicaid access to more people across states. Today, around 8% of the population is uninsured. The numbers are getting smaller, but that still accounts for around 26 million people.
What a lack of quality healthcare looks like in a person’s health
A first-time pregnant woman in rural Idaho loses access to prenatal care when her local health clinic closes its OB/GYN division. Now, she and her partner must travel to a neighboring county for care. This stresses and strains the couple as transportation costs mount and more time off is needed to cover longer appointment times.
On top of that, all their town’s women need reproductive care, overloading medical facilities in neighboring counties and making it harder to reschedule appointments. Without easy access to reliable care, the pregnant woman is at a greater risk of pregnancy, delivery, and postpartum complications should issues arise.
Neighborhood and built environment
One’s neighborhood and the built environment are social drivers of health that encompass public safety and the availability of safe, stable housing and transportation, walkable streets, accessible recreation facilities, clean drinking water, and nutritious and fresh food. With this social driver, it may be common to see the snowball effect of one factor, both positive and negative, influencing many others.
What a lack of built environments looks like in a person’s health
Tenants in a big city rent from a landlord whose units are in disrepair, exposing people to health hazards like mold and poor heating and cooling systems. On top of that, the city’s air is polluted, increasing cases of respiratory illness and exasperating chronic conditions among tenants.
Even those who can see doctors can’t find permanent relief due to everyday conditions. Appeals to the landlord go unanswered, leading to a sense of powerlessness and increased stress. Those who have the means to move may struggle to find suitable housing near their places of work and within their budgets.
Social and community context
Social and community contexts are social drivers of health that encompass social relationships, family and communal support systems, community engagement, discrimination, and stress. This social driver may be the hardest to detect physically, with a lack of resources or social and creative outlets largely affecting mental health outcomes.
What social and community context looks like in a person’s health
A young man openly practices his Islamic faith. He likes his co-workers, but they make inappropriate comments when he excuses himself for mid-day prayers. The Islamic community in his city is small, and he finds it hard to gather in public due to fear of prejudice.
When the young man’s car is broken into one night, he hesitates to call the police, fearing they’ll treat him with hostility or won’t take his needs seriously. Tense social relationships and a lack of community support make the young feel isolated, affecting his ability to cope with stress and make meaningful connections.
How unaddressed social drivers affect health outcomes
The examples above may feel extreme. After all, what parent, teacher, colleague, or doctor wouldn’t recognize and attempt to remedy the ill effects of a lack of employment or education?
The sad reality is a person’s health is likely to slip through the cracks when social drivers aren’t addressed or when a person doesn’t have the network, resources, experience, age, or know-how to act in their own best interest.
Treating people for aches and pains alone only manages the symptoms of greater issues. This can drive up individual and hospital healthcare costs as health relapses lead to readmissions and greater utilization of medical resources. Without intervention at the root cause, the cost and prevalence of health-related challenges increase, further deteriorating widespread community health.
How CBOs and community health workers improve health outcomes by addressing social drivers
Community-based organizations (CBOs), community health workers (CHWs), and other community-based providers work to address the root cause of a client’s health condition or personal circumstances. These providers tackle the social drivers of health at their source, treating the whole person (and not only their diagnosis), and changing individual and community health outcomes for the better.
With this in mind, let’s reimagine our previous scenario with CBO and CHW intervention.
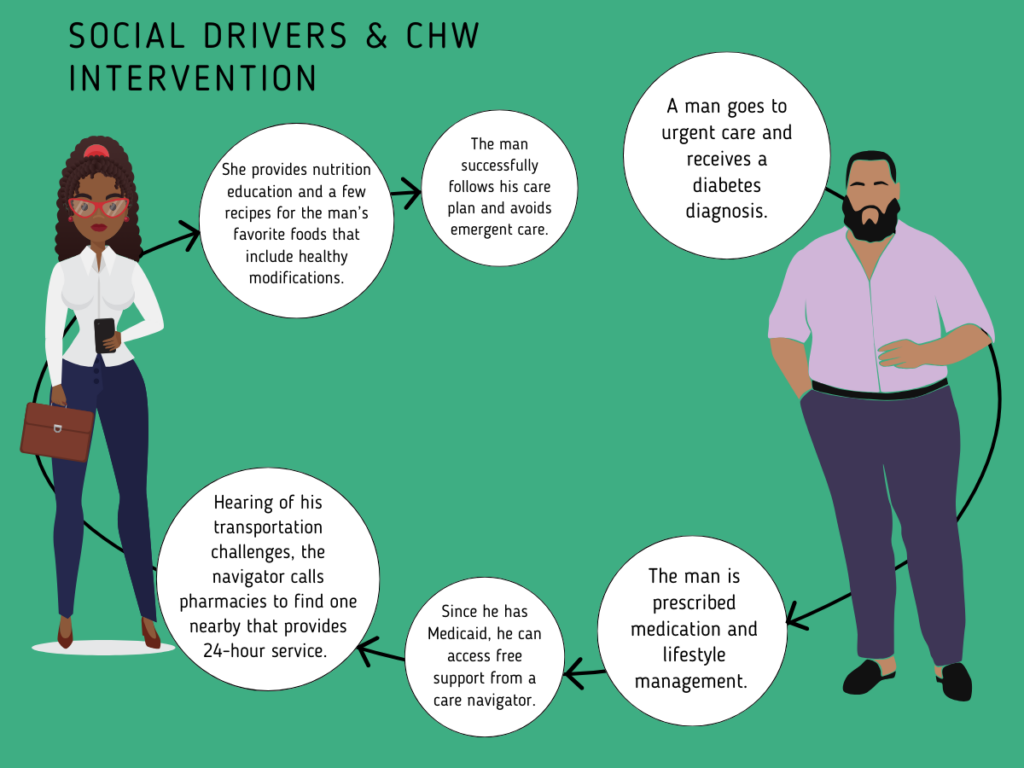
A man receives a type 2 diabetes diagnosis after years of experiencing symptoms. Since the man’s family has Medicaid, he qualifies for free support from a community health worker. At checkout, the man is referred to a community resource center to get support.
The man is connected with a care navigator. The navigator follows up about the man’s care plan. The man mentions that he’s had trouble picking up his prescriptions because of transportation challenges due to using a shared vehicle. The navigator calls around to pharmacies, finding one nearby that provides 24-hour service and free delivery.
The same care navigator sees that the man was recommended to make diet changes, so she offers education and a few recipes for his favorite foods that include healthy modifications. The man has successfully followed his care plan, and his immediate family members also have experienced positive health outcomes.
With the guidance from the Centers for Medicare and Medicaid Services (CMS) for healthcare facilities to drive the adoption of strategies that address social determinants of health, as well as increasing opportunities for Medicaid reimbursement for services provided by CHWs, incorporating SDOHs into a person’s care is becoming more commonplace.
For each social driver of health, there’s no doubt an organization within proximity to a client that can address challenges and promote social resources. While one organization helps clients in poorly maintained buildings file complaints with their city to get units fixed, others help tenants find rent relief in the face of a job loss.
Community-based providers within CBOs and nonprofits work with schoolteachers and guidance counselors to provide free or low-cost tutoring programs or nature-based anxiety and stress management sessions with kids and teens. Local fitness centers partner with faith-based CBOs to facilitate in-person and virtual hangouts for people who share religious beliefs.
As clinical and community-based providers shift to working closer together to provide whole-person care, the idea of “drivers” versus “determinants” is more appropriate. SDOHs will no longer seem to predetermine a client’s outcomes. Instead, they simply will be non-medical factors that, with the empathetic support from experienced community health workers, can be addressed to improve the quality of lives and long-term health outcomes of clients.




