Community health workers (CHWs) are essential to California’s healthcare landscape. They bridge the gap between communities and the healthcare system, addressing social drivers of health to improve the health and quality of life of community members.
Recognizing this, the California Department of Health Care Services (DHCS) added Community Health Worker (CHW) services as a Medi-Cal benefit. California is one of 24 states that has allowed community health workers to file for Medicaid (or Medi-Cal in California) reimbursement for their services. With the approval of a CHW benefit, CHWs and community-based organizations (CBOs) can improve the reach and impact of their services by billing Medi-Cal and creating revenue from the whole-person care work they do every day.
Learn the necessary steps CHWs and CBOs with CHWs must take to take advantage of billing through Medi-Cal managed care organizations (MCOs).
Understand Eligible Services
First, not all services can be reimbursed through Medi-Cal. Tasks such as client management and data input are not eligible for billing. Eligible activities are those that address social drivers of health, where CHWs directly support clients and community members, such as social care navigation, health education, screenings and assessments, and advocacy.
-
Health navigation: Providing information, training, referrals, or support to improve access to healthcare or addressing barriers to care by arranging transportation or translation/interpretation services.
-
Health education: Addressing social drivers of health to improve physical and mental health care, including providing information or instruction on health topics.
-
Social needs screening and assessment: Connecting Medi-Cal members to appropriate services to improve their health.
-
Individual support or advocacy: Assisting a Medi-Cal member in preventing the onset or worsening of a health condition or preventing injury or violence.
Meet the Medi-Cal Qualifications to Bill as a Community Health Worker

A community health worker is a trusted member of the community who typically works or volunteers in the role because they have lived experience. Lived experience for a CHW is personal experiences that align with the community population they’re serving (e.g., a CHW has experienced homelessness and helps community members access safe housing).
Any CHW can provide preventative services that address social drivers of health. However, for those services to be eligible for Medi-Cal reimbursement, the CHW must meet the minimum work experience requirement or have a CHW certificate.
New CHWs, without work experience, who want to bill this Medi-Cal benefit must complete a CHW certificate program that includes core curriculum and a field experience component.
A person with 2,000 hours of experience working as a CHW in paid or volunteer positions within the previous three years does not need to complete training before they start billing for services. However, they must complete CHW certificate training program within 18 months to continue to bill.
Enroll as a Medi-Cal Provider
First, if there is an eligible pathway for you or your organization to enroll as a Medi-Cal provider, you must do so on the Provider Application and Validation for Enrollment (PAVE) website. An individual CHW also has the option to join a Supervising Provider or hub and provide services under their credentials.
Contract with your Local Managed Care Organization (MCO)
Next, your Supervising Organization must contract with the managed care organization(s) (MCO), or health plans, in your area.
Since every MCO’s coverage area is different, determine which health plans you or your organization must credential with based on your county. Along with the application, you’ll need to submit proof of credentials, business licenses, and any other relevant documentation required by the local MCO.
Pear Suite has completed these applications and are an in-network provider for nearly a dozen local and regional health plans throughout California. If you are a CHW or CHW employer, such as an outreach nonprofit or agency, and would like support, reach out for help with this process.
You may also join the Pear Cares Provider Network, if you would rather bill through our contracts and use our clinical, supervising, and billing support. Schedule a demo and see how it works.
Establish an Operating System
You likely already document care plans, referrals, education provided, and other interactions with clients and community members on paper or in databases or spreadsheets. When submitting information for reimbursement, ensuring that these notes and other documents are together is crucial. And because managing this entire process can be cumbersome, organizations and CHWs are encouraged to invest in an operating system to create efficient workflows, safely secure and share sensitive data, generate and manage claims, and meet other compliance requirements.
As of June 2024, start-up funding is available to organizations in select counties who are interested in partnering with Pear Suite to bill for CHW services. Have questions or want to find out if your organization qualifies? Schedule a call.
When looking for an operating system to support CHW services, find an all-in-one solution with a client records system, assessment and communication tools, and claims management capabilities that can specifically handle Medi-Cal’s billing requirements. This will save you and your team from having multiple systems and needing to figure out how to transfer documentation from one to the other.
Learn the Medi-Cal Billing Codes
Get comfortable with the specific Medi-Cal billing codes for CHW services.
Some common codes and rates include:
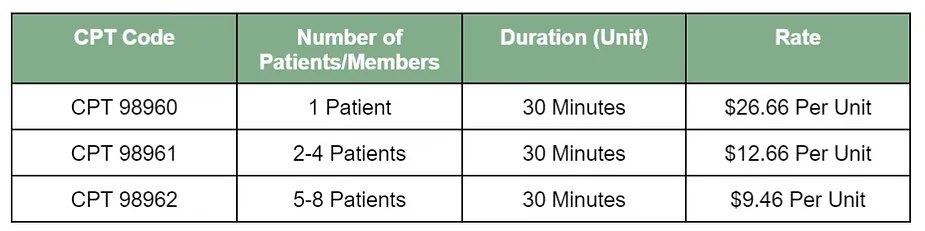
(These rates may vary as some MCOs offer higher rates.)
Reimbursements are made based on the number of units completed, and each unit equals 30 minutes. The maximum allowance per day per Medi-Cal member is four units (or two hours) for any service provider.
Understand Medi-Cal Member Eligibility
Medi-Cal will only reimburse CHWs and CBOs for care provided to eligible members who meet certain requirements. The qualifications are broad, but you’ll want to make sure the member is eligible on the date of service.
Along with active enrollment in Medi-Cal through an MCO, CHW services also must be considered medically necessary as the member qualifies with one or more of the following:
-
Diagnosis of one or more chronic health (including behavioral health) conditions, or a suspected mental disorder or substance use disorder that has not yet been diagnosed.
-
Presence of medical indicators of rising risk of chronic disease (e.g., elevated blood pressure, elevated blood glucose levels, elevated blood lead levels or childhood lead exposure, etc.) that indicate risk but do not yet warrant diagnosis of a chronic condition.
-
Any stressful life event presented via the Adverse Childhood Events screening.
-
Presence of known risk factors, including domestic or intimate partner violence, tobacco use, excessive alcohol use, and/or drug misuse.
-
Results of a social drivers of health (SDOH) screening indicating unmet health-related social needs, such as housing or food insecurity.
-
One or more visits to a hospital emergency department (ED) within the previous six months.
-
One or more hospital inpatient stays, including stays at a psychiatric facility, within the previous six months, or being at risk of institutionalization.
-
One or more stays at a detox facility within the previous year.
-
Two or more missed medical appointments within the previous six months.
-
Expressed need for support in health system navigation or resource coordination services.
-
Need for recommended preventive services, including updated immunizations, annual dental visits, and well childcare visits for children.
-
Chronic health conditions or is at risk for chronic health conditions, including behavioral health.
A complete list of conditions and eligibility requirements is available from the California Department of Health Care Services.
Once you’re qualified to bill for CHW services, you or your CBO are well on their way to creating sustainable revenue. With the additional stability, many organizations have shared that they’ve been able to free themselves from continually chasing other revenue streams, such as grants and donations, and be able to shift their focus to providing more needed services to community members. This is the intent of the CalAIM program: To involve community-based organizations and incentivize addressing social drivers of health to promote whole-person care.




